The author on the tricky balance between Prozac and sunlight.
Mood music for this post: “Times Like These” by The Foo Fighters:
[youtube=http://www.youtube.com/watch?v=rhzmNRtIp8k&hl=en_US&fs=1&]
This post is a sequel to Prozac Winter, which I wrote back in January.
Back then, I was experiencing some hefty mood swings, which is pretty normal for me at the start of winter. I was listening Nine Inch Nails a lot, which is never a good sign.
My therapist and a woman I’ll call Dr. Prozac (she’s the anti-depressant specialist who works with my therapist) upped by dosage by 20 mg. for the duration of winter, which worked remarkably well. On balance, I had a pretty good winter. It turns out that winter, with it’s cold temperatures and shorter spans of daylight, knocks my brain chemistry out of alignment. It’s actually a very common problem. The sun provides nutrients the brain needs to function properly.
Now we’re approaching summer, with longer days, hot weather and all the rays I need. So my dosage is being rolled back to where it was before the winter.
I have to drive an hour to Dr. Prozac this morning so she can measure my progress. She’s done a great job up to this point. While I’m down there, I’ll go have lunch with a dear friend I haven’t seen in awhile.
It’s all good.
I’ve gotten a fair amount of questions about the true value of anti-depressants. I’m not a doctor, so don’t take my perspective as Gospel. Also remember there’s no one-size-fits-all solution here. What I write here is based on my own personal experiences. What works for me may not work for the next person.
The more I read up on depression, mental illness and the drugs prescribed for it, the more I see the human brain as an engine. Comparing it to an engine makes this whole think easier to understand.
We know that the engine of a car is made up of many small parts and when one part gets worn out the rest of the engine can fail. We know that a car needs just the right amount of oil, transmission fluid, brake fluid etc. to function properly. If the oil runs out, the engine seizes up. If the brake fluid runs dry, the breaks fail. On the flip side, too much of these fluids can harm the engine.
We also know that the auto mechanic uses many different techniques to keep engines healthy or fix them when they break.
The brain works much the same way.
![[ImgPet.jpg]](https://theocddiaries.com/wp-content/uploads/2012/04/imgpet.jpg?w=300)
Think of the different drugs as different tools to deal with very specific problems in the engine.
In my case, Prozac addresses the very specific fluid deficiencies that spark OCD behavior. The effect is not as simple as the image below suggests (though I do like the image and need to find the artist so I can properly credit him/her):
It may also be useful to think of the therapist as the auto mechanic who is well versed in how to regulate the different engine fluids and pinpoint specific fixes for specific problems. It’s also true that there are good mechanics and bad mechanics who sometimes make the problem worse.
In the brain, when certain fluids are running low, the engine stops working properly. The result is depression and a host of other mental disorders.
Since OCD is essentially the brain pumping and spinning out of control, I like to think of my specific problem as a lack of brake fluid.
But the good folks at WebMD explain it much better than I ever could. Here’s some WebMD wisdom I included in Prozac Winter:
How Antidepressants Work
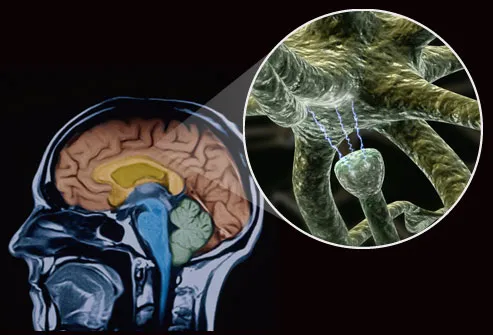
Most antidepressants work by changing the balance of brain chemicals called neurotransmitters. In people with depression, these chemicals are not used properly by the brain. Antidepressants make the chemicals more available to brain cells like the one shown on the right side of this slide:
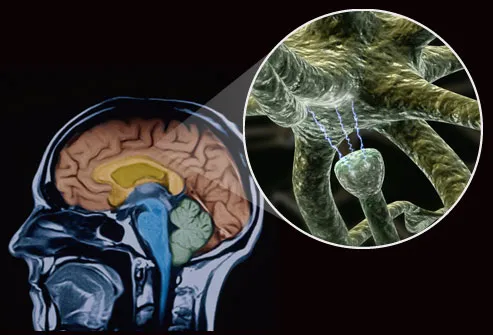
Antidepressants can be prescribed by primary care physicians, but people with severe symptoms are usually referred to a psychiatrist.
Realistic Expectations
In general, antidepressants are highly effective, especially when used along with psychotherapy. (The combination has proven to be the most effective treatment for depression.) Most people on antidepressants report eventual improvements in symptoms such as sadness, loss of interest, and hopelessness.
But these drugs do not work right away. It may take one to three weeks before you start to feel better and even longer before you feel the full benefit.
And, just as weather can impair the performance of your car engine (myfather‘s car went for a swim when Revere got flooded out in The Blizzard of 1978 and never worked properly again), too much bad weather can keep the brain from working properly:
Why do I seem to get so gloomy each winter, or sometimes beginning in the fall?
You may have what’s called seasonal affective disorder, or SAD. The condition is marked by the onset of depression during the late fall and early winter months, when less natural sunlight is available. It’s thought to occur when daily body rhythms become out-of-sync because of the reduced sunlight.
Some people have depression year round that gets worse in the winter; others have SAD alone, struggling with low moods only in the cooler, darker months. (In a much smaller group of people, the depression occurs in the summer months.)
SAD affects up to 3% of the U.S. population, or about 9 million people, some experts say, and countless others have milder forms of the winter doldrums.
So this worsening of mood in the fall and winter is not just my imagination?
Not at all. This “winter depression” was first identified by a team of researchers at the National Institute of Mental Health in 1984. They found this tendency to have seasonal mood and behavior changes occurs in different degrees, sometimes with mild changes and other times severe mood shifts.
Symptoms can include:
- Sleeping too much
- Experiencing fatigue in the daytime
- Gaining weight
- Having decreased interest in social activities and sex
SAD is more common for residents in northern latitudes. It’s less likely in Florida, for instance, than in New Hampshire. Women are more likely than men to suffer, perhaps because of hormonal factors. In women, SAD becomes less common after menopause.
I’m still learning the science of mental illness, and remember I’m not a doctor. I just share my personal experiences and explain what works for me.
Class dismissed.
![[ImgPet.jpg]](https://theocddiaries.com/wp-content/uploads/2012/04/imgpet.jpg?w=300)