Depression has claimed another victim. Published reports confirm that legendary guitarist Ronnie Montrose’s March 3 death was a suicide.
Many of you are unfamiliar with him, but his playing left a lasting mark on a lot of mega-star musicians, including Eddie Van Halen, who recorded four studio albums with original Montrose singer Sammy Hagar.
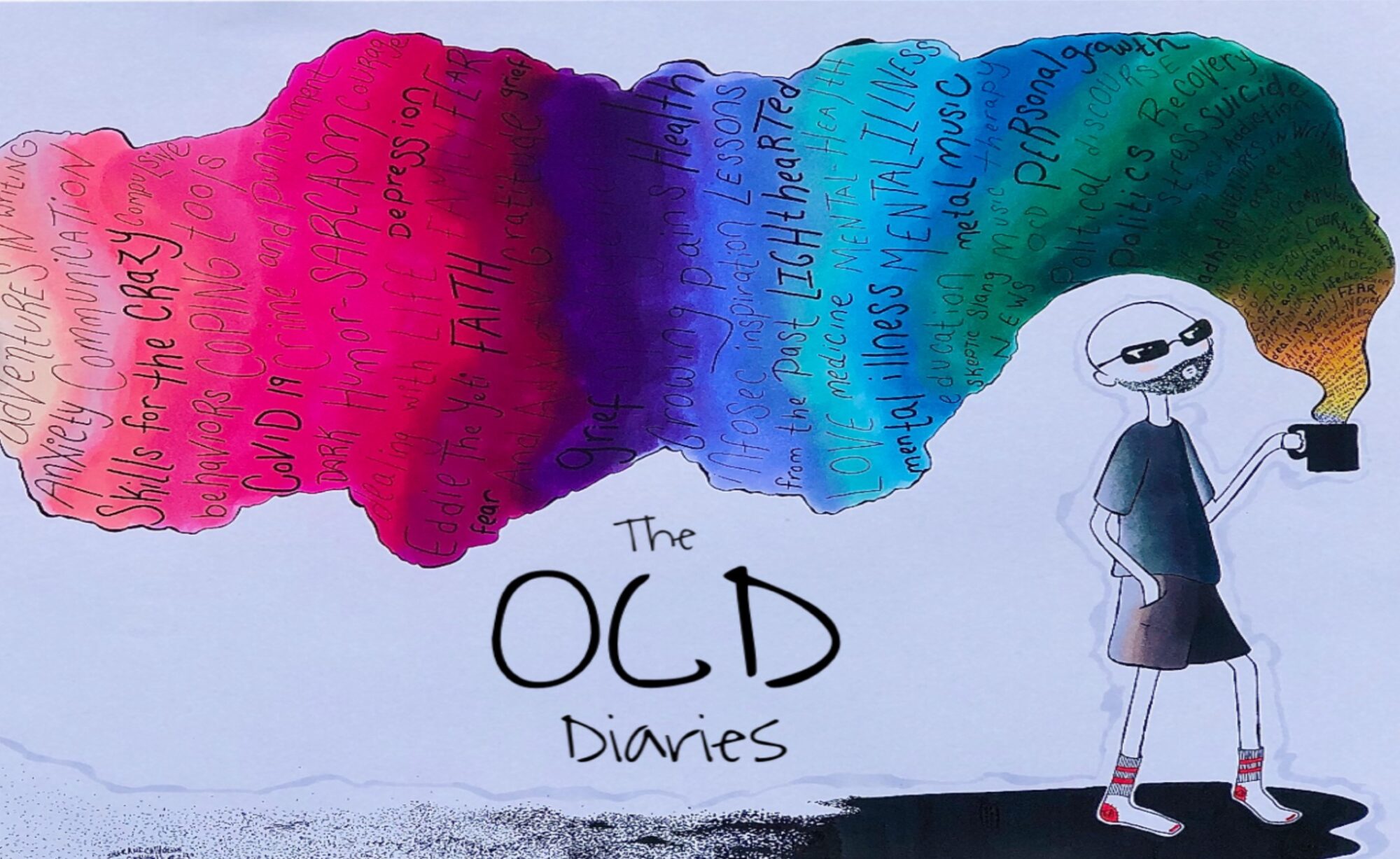
Mood music:
Montrose’s wife, Leighsa Montrose, described how badly he suffered in an interview with Guitar Player magazine:
“Ronnie had a very difficult childhood, which caused him to have extremely deep and damaging feelings of inadequacy,” said Leighsa. “This is why he always drove himself so hard. He never thought he was good enough. He always feared he’d be exposed as a fraud. So he was exacting in his self criticism, and the expectations he put upon himself were tremendous. Now I see that perhaps he didn’t want to carry these burdens for very much longer.”
I’ve been ultra-sensitive on the issue of suicide ever since my best friend took his life 15-plus years ago.
I was angry with him for many years. I thought he was a coward who left behind a mess. My thinking has evolved considerably since then. I now see suicide for what it is: The act of a person so ill with depression that they’ve lost the ability to think clearly. Whenever I hear of a suicide, I feel the need to mention it here because I don’t want anyone else’s name tarnished because that’s how it ended for them.
The topic is a tough one for Catholics like me, because we were always taught that suicide is a ticket straight to Hell. These lines from the Catechism of the Catholic Church show that suicide isn’t the trip to eternal damnation many in the church would have us believe:
“2282 Grave psychological disturbances, anguish, or grave fear of hardship, suffering, or torture can diminish the responsibility of the one committing suicide.
2283 We should not despair of the eternal salvation of persons who have taken their own lives. By ways known to him alone, God can provide the opportunity for salutary repentance. The Church prays for persons who have taken their own lives.”
Nothing is ever as black and white as we’d like to believe. The older I get, the clearer that point becomes.
It used to seem strange to me how depression could snuff out one life while leaving legions more intact. But it’s not so strange, really. Cancer kills a lot of people every day, but many more are left standing.
I’m no stranger to depression. I suffer the bleak feelings of it regularly, though never to the point of suicide. Mine is a brooding, curmudgeonly form of depression that I’ve learned to manage well through therapy and medication.
I’m one of the lucky ones, I suppose. I’ll just be grateful about it and leave it at that.
I hope Montrose finds the peace he couldn’t find in life.





 As for that other OCD segment on NPR,
As for that other OCD segment on NPR, 


